
Table of Contents


Composite Injection Molding: 5 Transformative Benefits for Effective Smile Restoration
Dental Composite: 5 Stunning Benefits for Effective Smile Enhancement

Teeth Bleaching: 5 Radiant Benefits for Effective Smile Brightening

Dental Veneer: 5 Stunning Benefits for Effective Smile Enhancement
Implant-Supported Fixed Prostheses: 5 Advanced Benefits for Effective Smile Restoration
Root Canal Treatment: Preserving Natural Teeth Through Specialized Endodontic Care
Root canal treatment, a cornerstone of endodontics, is a specialized dental procedure designed to save a tooth with infected or damaged dental pulp—the soft tissue inside the tooth containing nerves, blood vessels, and connective tissue. By removing the compromised pulp, cleaning and disinfecting the tooth’s interior, and sealing it with biocompatible materials, root canal therapy alleviates pain, prevents infection spread, and preserves the natural tooth. This article explores the definition, indications, procedure, aftercare, benefits, myths, and future advancements of root canal treatment, emphasizing its critical role in restorative dentistry.
Defining Root Canal Treatment
Root canal treatment, often referred to as endodontic therapy, addresses issues within the dental pulp caused by deep decay, trauma, cracks, or repeated dental procedures. Affecting millions annually (e.g., 15 million root canals performed in the U.S. each year), pulp infections or inflammation can lead to severe pain, abscesses, or tooth loss if untreated. The procedure involves removing the affected pulp, cleaning the root canal system, and sealing it with materials like gutta-percha, followed by restoration to restore function and aesthetics. Root canal treatment is a highly effective solution, with success rates exceeding 90% over 10 years, per clinical studies, allowing patients to retain their natural teeth.
Indications for Root Canal Treatment
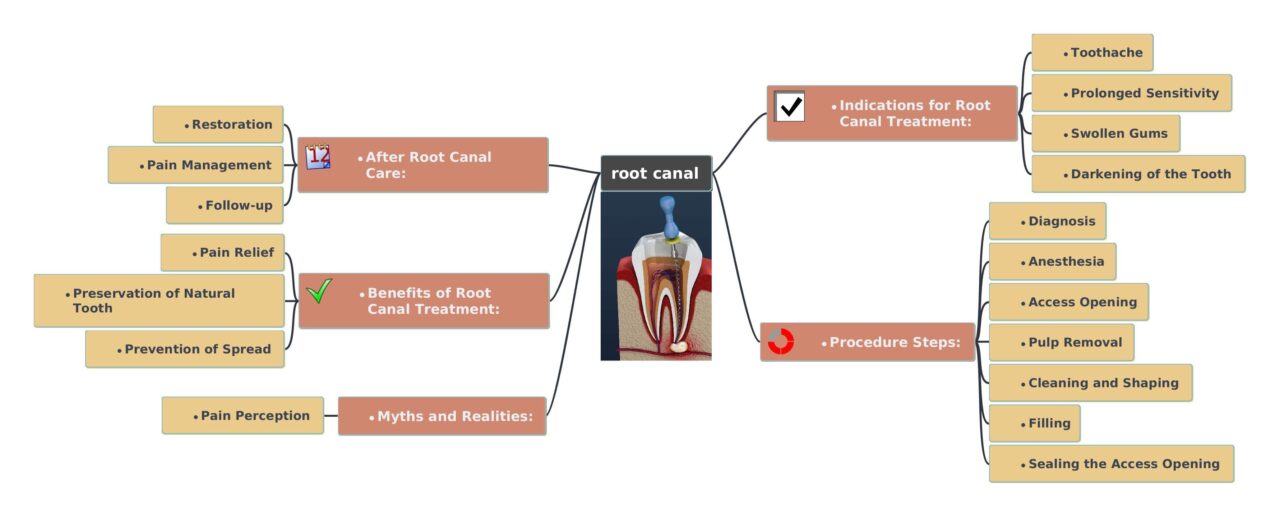
Prompt recognition of symptoms is essential for timely intervention. Common indications include:
- Severe Toothache: Persistent or intense pain, especially when chewing or applying pressure, indicating pulp inflammation or infection.
- Prolonged Sensitivity: Lingering discomfort to hot, cold, or sweet stimuli, even after removal of the trigger.
- Swollen Gums: Tenderness, swelling, or redness in the gums near the affected tooth, often signaling an abscess.
- Tooth Discoloration: Darkening or graying of the tooth, suggesting pulp necrosis or internal bleeding.
- Gingival Abscess: Recurring or persistent pimples on the gums, indicating underlying infection.
These symptoms may reflect irreversible pulpitis or pulp necrosis, necessitating root canal treatment to prevent complications like periapical abscesses or bone loss.
Root Canal Procedure Steps
Root canal treatment is a multi-step, specialized process performed under local anesthesia to ensure patient comfort:
- Diagnosis: The dentist conducts a clinical examination, reviews symptoms, and uses diagnostic tools like X-rays or cone-beam CT to assess pulp damage and canal anatomy. Tests like percussion or thermal sensitivity confirm the need for treatment.
- Anesthesia: Local anesthesia numbs the tooth and surrounding tissues, ensuring a pain-free experience.
- Access Opening: A small opening is drilled into the tooth’s crown to access the pulp chamber, often using a dental dam for isolation and hygiene.
- Pulp Removal: The infected or damaged pulp is removed from the pulp chamber and root canals using specialized instruments like endodontic files.
- Cleaning and Shaping: The canals are cleaned, disinfected with solutions like sodium hypochlorite, and shaped to prepare for filling, ensuring all debris and bacteria are eliminated.
- Filling: The cleaned canals are filled with gutta-percha, a biocompatible material, to seal the space and prevent reinfection.
- Sealing the Access Opening: The access cavity is sealed with a temporary or permanent filling, such as composite resin, to protect the tooth.
- Restoration: A dental crown or permanent filling is often placed to strengthen the tooth and restore its function and appearance.
After Root Canal Care
Post-treatment care is crucial for long-term success:
- Oral Hygiene: Brush twice daily with fluoride toothpaste and floss to prevent secondary decay or infection.
- Avoid Hard Foods: Refrain from chewing hard or sticky foods (e.g., nuts, toffees) to protect the restoration.
- Pain Management: Mild discomfort for 1–3 days post-procedure can be managed with over-the-counter medications like ibuprofen.
- Follow-Up Visits: Regular dental check-ups (every 6–12 months) monitor the treated tooth and ensure healing.
- Protective Measures: Use a mouthguard for sports or if bruxism (teeth grinding) is present to prevent fractures.
Benefits of Root Canal Treatment
Root canal therapy offers significant advantages:
- Pain Relief: Eliminates toothache and discomfort from pulp infection or inflammation.
- Tooth Preservation: Saves the natural tooth, avoiding extraction and maintaining oral function and aesthetics.
- Infection Control: Prevents the spread of infection to surrounding tissues, teeth, or systemic circulation.
- Restored Function: Allows normal chewing and biting, enhancing quality of life.
- Cost-Effectiveness: Often more economical than extraction followed by implants or bridges ($800–$1,500 vs. $3,000–$5,000 in the U.S.).
Myths and Realities
Common misconceptions about root canal treatment include:
- Myth: Root Canals Are Painful: Modern anesthesia and techniques make the procedure as comfortable as a routine filling.
- Myth: Root Canals Cause Illness: No scientific evidence links root canals to systemic diseases; they are safe and effective.
- Myth: Extraction Is Better: Preserving the natural tooth maintains jawbone health and avoids costly replacements.
Challenges and Considerations
Challenges include:
- Complexity: Anatomical variations (e.g., curved or calcified canals) require specialized skills and tools like dental operating microscopes.
- Success Rates: While high (90–95%), failures can occur due to reinfection, missed canals, or fractures, necessitating retreatment or apicoectomy.
- Patient Anxiety: Fear of the procedure, fueled by myths, may delay treatment. Patient education and sedation options can help.
- Restoration Needs: Post-treatment crowns add cost and require maintenance to ensure durability.
Future Innovations
Endodontics is advancing with technology:
- Digital Tools: Cone-beam CT and digital apex locators improve canal navigation and precision.
- Laser Disinfection: Laser-assisted techniques enhance bacterial elimination in complex cases.
- Regenerative Endodontics: Stem cell therapies and bioactive materials may regenerate pulp tissue, especially in pediatric cases.
- AI Diagnostics: AI tools may predict treatment outcomes or identify canal anomalies.
Conclusion
Root canal treatment is a specialized, highly effective procedure in endodontics, preserving natural teeth by addressing pulp infections or damage. By alleviating pain, preventing infection spread, and restoring function, it enhances oral health and quality of life. With proper care and advancements in digital and regenerative technologies, root canal therapy remains a cornerstone of restorative dentistry. Patients experiencing symptoms should consult a certified endodontist or visit American Association of Endodontists for more information.
- American Association of Endodontists. (2025). Root Canals.
- American Dental Association. (2025). Root Canal Treatment.
- Torabinejad, M., et al. (2017). Regenerative Endodontics: A Review. Journal of Endodontics, 43(9), S16–S31.
- American Association of Endodontists. (2025). Endodontic Treatment Options.
