
Table of Contents


Composite Injection Molding: 5 Transformative Benefits for Effective Smile Restoration
Dental Composite: 5 Stunning Benefits for Effective Smile Enhancement

Teeth Bleaching: 5 Radiant Benefits for Effective Smile Brightening

Dental Veneer: 5 Stunning Benefits for Effective Smile Enhancement
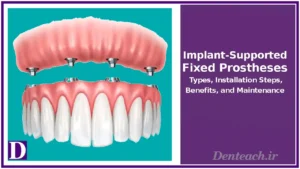
Implant-Supported Fixed Prostheses: 5 Advanced Benefits for Effective Smile Restoration

Dental Occlusion: The Foundation of a Healthy Bite and Smile
Dental occlusion refers to the alignment and contact of upper and lower teeth during biting, chewing, or resting, a critical factor in oral health, function, and aesthetics. Misaligned occlusion, or malocclusion, affects approximately 60–75% of the population to varying degrees, per the American Association of Orthodontists (AAO), leading to issues like tooth wear or jaw pain. Proper occlusion ensures efficient chewing, clear speech, and facial harmony, while addressing issues early prevents complications. This article explores the definition, importance, types, anatomical context, treatments, challenges, and future trends of dental occlusion, emphasizing its role in comprehensive dental care.
Defining Dental Occlusion
Dental occlusion describes how upper and lower teeth align and interact when the jaws close, influenced by tooth positioning, jaw structure, and temporomandibular joint (TMJ) function. An ideal occlusion distributes chewing forces evenly, minimizing stress on teeth, gums, and jaw muscles. It involves static (resting bite) and dynamic (chewing or speaking) relationships, assessed through dental exams, X-rays, or digital scans. Proper occlusion enhances oral function, while malocclusion—present in 20–30% of adults with significant issues—can lead to dental and systemic problems, necessitating intervention for optimal health.
Importance of Dental Occlusion
Proper occlusion is vital for multiple reasons:
- Chewing Efficiency: Well-aligned teeth enable effective mastication, aiding digestion and nutrient absorption, critical for overall health.
- Speech Clarity: Correct occlusion supports tongue and lip movements, improving articulation and reducing speech issues in 10% of malocclusion cases.
- Prevention of Dental Issues: Proper alignment prevents excessive tooth wear, fractures, gum recession, and TMJ disorders, which affect 15% of adults with malocclusion.
- Aesthetics: An ideal bite enhances smile symmetry and facial balance, boosting confidence in 80% of patients post-treatment, per AAO data.
- Systemic Health: Proper occlusion reduces strain on jaw muscles, lowering risks of headaches or neck pain linked to TMJ issues.
Anatomical and Morphological Context
Occlusion is deeply tied to dental and jaw anatomy:
- Tooth Structure: The morphology of cusps, fossae, and occlusal surfaces determines how teeth interdigitate. For example, molar cusps align to maximize chewing efficiency.
- Jaw Alignment: The maxilla and mandible’s skeletal relationship, influenced by bone growth, affects occlusion types (e.g., Class I, II, III).
- TMJ Function: The temporomandibular joint’s hinge and sliding movements facilitate dynamic occlusion, with misalignment causing dysfunction in 5–10% of cases.
- Dental Arches: The curvature and spacing of dental arches impact tooth alignment, with crowding or spacing contributing to malocclusion in 25% of patients.
This anatomical focus justifies including anatomy-and-morphology in the Wiki Categories, as occlusion directly relates to tooth and jaw structure.
Types of Dental Occlusion
Occlusion types vary based on tooth and jaw alignment:
- Class I Occlusion (Neutrocclusion): The ideal bite, where upper teeth slightly overlap lower teeth, with the first molar’s mesiobuccal cusp aligning with the lower molar’s buccal groove. Occurs in 50–55% of the population.
- Class II Occlusion (Distocclusion): Known as an overbite, where upper teeth significantly protrude over lower teeth, often due to a retruded mandible. Affects 15–20% of individuals, increasing risks of tooth wear.
- Class III Occlusion (Mesiocclusion): Known as an underbite, where lower teeth extend beyond upper teeth, often due to a protruded mandible. Seen in 5–10% of cases, impacting aesthetics and function.
- Crossbite: Upper teeth sit inside lower teeth, affecting anterior or posterior teeth, causing misalignment in 10% of patients.
- Open Bite: Teeth fail to meet when jaws close, often due to habits like thumb-sucking, affecting 5% of children.
- Overjet: Excessive horizontal overlap of upper teeth, distinct from overbite, complicating chewing in 10% of cases.
Oral and maxillofacial surgery
Treatment of Dental Occlusion Issues
Treatments address malocclusion based on severity:
- Orthodontic Treatment: Braces or clear aligners (e.g., Invisalign) correct alignment over 12–36 months, effective in 90% of cases for Class I and II malocclusions.
- Occlusal Adjustments: Selective grinding or reshaping of tooth surfaces improves bite harmony, used in 20% of minor malocclusion cases.
- Restorative Dentistry: Crowns, bridges, or implants restore worn or missing teeth, correcting occlusion in 15% of severe cases.
- Surgical Intervention: Orthognathic surgery repositions jaws for Class III or severe skeletal issues, with a 95% success rate for functional improvement.
- TMJ Therapy: Splints or physical therapy manage TMJ disorders linked to malocclusion, reducing pain in 70% of patients.
Challenges and Considerations
Challenges include:
- Cost: Treatments range from $3,000–$7,000 for orthodontics to $20,000 for surgery, with partial insurance coverage.
- Treatment Duration: Orthodontics or surgery may take years, impacting patient compliance in 20% of cases.
- Discomfort: Braces or adjustments cause temporary soreness, affecting 30% of patients.
- Complexity: Severe malocclusions require multidisciplinary care (e.g., orthodontists, surgeons), complicating treatment plans.
- Maintenance: Long-term retainer use is needed post-treatment to prevent relapse in 25% of cases.
Future Trends
Occlusion management is advancing:
- Digital Orthodontics: 3D scans and AI-driven treatment planning improve precision, reducing treatment time by 15%.
- Clear Aligners: Advanced materials enhance aligner comfort and effectiveness, popular in 40% of orthodontic cases.
- Minimally Invasive Adjustments: Laser-based reshaping reduces the need for extensive grinding.
- Regenerative Therapies: Bioactive materials may repair worn enamel, improving occlusal surfaces.
Conclusion
Dental occlusion is a cornerstone of oral health, influencing chewing, speech, aesthetics, and systemic well-being. By understanding occlusion types and addressing malocclusion through orthodontics, restorative treatments, or surgery, dental professionals ensure optimal outcomes. With advancements like digital orthodontics and minimally invasive techniques, occlusion management is more effective than ever. Patients seeking bite correction should consult a dentist or orthodontist or visit American Association of Orthodontists for personalized care.
- American Association of Orthodontists. (2025). About Orthodontics.
- American Dental Association. (2025). Orthodontic Treatment.
- Proffit, W. R., et al. (2018). Contemporary orthodontics. American Journal of Orthodontics and Dentofacial Orthopedics, 153(5), 611–620.
- American Association of Oral and Maxillofacial Surgeons. (2025). Orthognathic Surgery.
