
Table of Contents


Composite Injection Molding: 5 Transformative Benefits for Effective Smile Restoration
Dental Composite: 5 Stunning Benefits for Effective Smile Enhancement

Teeth Bleaching: 5 Radiant Benefits for Effective Smile Brightening

Dental Veneer: 5 Stunning Benefits for Effective Smile Enhancement
Implant-Supported Fixed Prostheses: 5 Advanced Benefits for Effective Smile Restoration
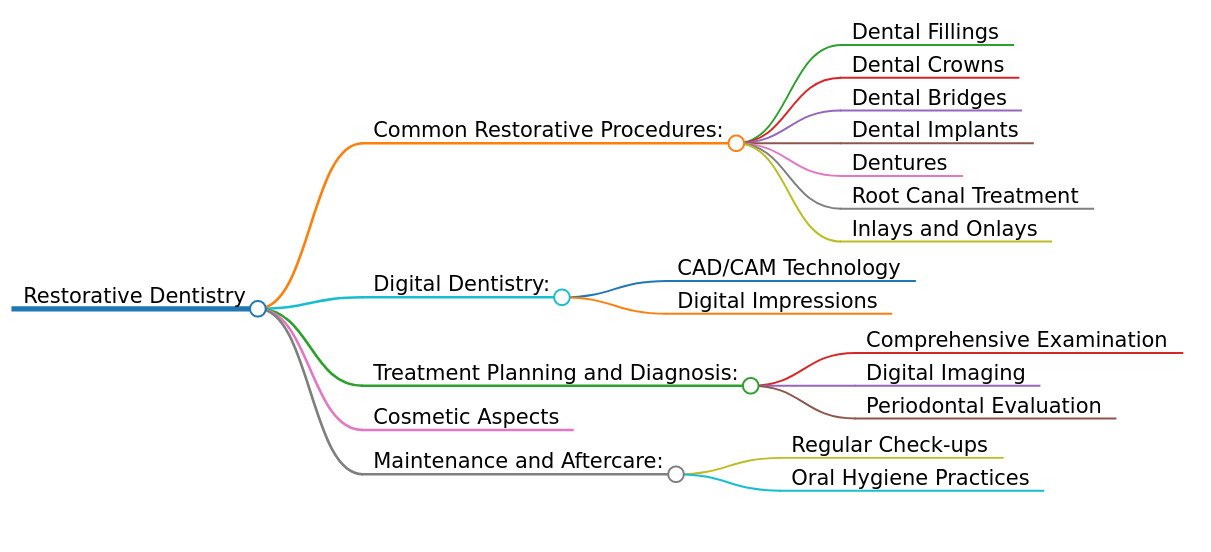
Restorative Dentistry: Revitalizing Smiles and Oral Health
Restorative dentistry is a vital branch of dentistry focused on repairing and replacing damaged or missing teeth to restore oral health, function, and aesthetics. Addressing issues like cavities, fractures, or tooth loss, which impact over 120 million Americans annually per the CDC, restorative procedures enhance quality of life by improving chewing, speaking, and smile confidence. From fillings to full mouth reconstructions, these treatments offer durable, tailored solutions. This article explores the definition, common procedures, benefits, consultation process, care, challenges, and future trends of restorative dentistry, highlighting its role in modern dental care.
Defining Restorative Dentistry
Restorative dentistry encompasses a range of procedures designed to repair or replace teeth affected by decay, trauma, or other conditions, restoring their form, function, and appearance. This specialty bridges general and cosmetic dentistry, addressing both health and aesthetic concerns. Using biocompatible materials like composite resin, porcelain, or titanium, restorative treatments prevent further oral health complications, such as tooth loss or gum disease, which affect 26% and 50% of adults, respectively. With a 90–95% success rate for procedures like crowns and implants over 10 years, restorative dentistry ensures lasting results for patients of all ages.
Common Restorative Dental Procedures
Restorative dentistry includes a variety of treatments tailored to specific needs:
- Dental Fillings: Treat cavities or minor damage using amalgam, composite resin, or glass ionomer, restoring tooth structure. Composite fillings are popular for their tooth-colored aesthetics.
- Dental Crowns: Custom-made caps cover damaged or weakened teeth, restoring shape and strength. Made from porcelain, zirconia, or metal, crowns last 10–15 years.
- Dental Bridges: Replace missing teeth by anchoring artificial teeth (pontics) to adjacent teeth or implants, preventing tooth shifting and restoring function.
- Dental Implants: Titanium posts surgically placed in the jawbone support crowns, bridges, or dentures, offering a permanent solution with a 95% success rate.
- Inlays and Onlays: Custom restorations for moderate damage, fitting within or over tooth cusps, made from porcelain or composite for durability and aesthetics.
- Dentures: Removable appliances replace multiple or all teeth, available as partial or complete sets, improving chewing and aesthetics.
- Root Canal Therapy: Removes infected pulp to save a tooth, followed by a crown or filling to restore strength, preventing extraction in 90% of cases.
- Full Mouth Reconstruction: Comprehensive plans address multiple issues (e.g., decay, missing teeth, bite problems), restoring entire oral function and aesthetics.
Benefits of Restorative Dentistry
Restorative dentistry offers significant advantages:
- Improved Oral Health: Prevents complications like decay progression, gum disease, or bone loss by addressing damage early.
- Enhanced Functionality: Restores chewing, biting, and speaking abilities, improving nutrition and communication.
- Aesthetic Enhancement: Creates natural-looking smiles, boosting confidence, with 85% of patients reporting satisfaction per the American College of Prosthodontists (ACP).
- Long-Lasting Results: Procedures like implants and crowns last 10–20 years with proper care, offering durable solutions.
- Systemic Health Benefits: Reduces risks of heart disease and diabetes complications linked to poor oral health.
Indications for Restorative Dentistry
Restorative treatments are recommended for:
- Tooth Decay: Cavities too extensive for simple fillings, requiring crowns or inlays.
- Tooth Damage: Cracks, fractures, or wear from trauma or grinding.
- Missing Teeth: Gaps impacting function, aesthetics, or jaw health, addressed by bridges, implants, or dentures.
- Post-Root Canal Care: Protecting treated teeth from fracture.
- Aesthetic Concerns: Discolored, misshapen, or uneven teeth affecting smile confidence.
The Restorative Dentistry Process
The restorative process is patient-centered:
- Consultation: The dentist assesses oral health using X-rays, intraoral scans, or exams to identify damage, decay, or tooth loss and discuss treatment goals.
- Treatment Planning: A personalized plan outlines procedures, materials, and timelines, often using digital tools like CAD/CAM for precision.
- Implementation: Procedures vary by treatment:
- Fillings: Decayed tissue is removed, and the cavity is filled.
- Crowns/Bridges: Teeth are prepared, impressions taken, and restorations cemented.
- Implants: Posts are surgically placed, followed by prosthetic attachment after healing (3–6 months).
- Dentures: Custom appliances are fitted and adjusted.
- Root Canal: Infected pulp is removed, and the tooth is sealed and restored.
- Follow-Up: Regular visits (every 6–12 months) monitor restoration integrity and oral health.
Caring for Restorative Treatments
Proper care ensures longevity:
- Oral Hygiene: Brush twice daily with fluoride toothpaste and floss to prevent decay around restorations.
- Regular Check-Ups: Dental visits every 6 months for cleanings and inspections, as 10–15% of restorations require maintenance within 10 years.
- Avoid Damaging Habits: Refrain from chewing hard objects (e.g., ice) to protect restorations.
- Healthy Diet: Limit sugary foods to reduce decay risk.
- Protective Measures: Use mouthguards for sports or bruxism to safeguard restorations.
Challenges and Considerations
Challenges include:
- Cost: Treatments range from $100–$500 for fillings to $3,000–$5,000 for implants, though insurance may offset costs.
- Time Commitment: Complex procedures like implants or full mouth reconstruction require multiple visits or months for completion.
- Maintenance: Diligent hygiene is critical to prevent failure, with 10–20% of restorations needing replacement within 10 years.
- Sensitivity: Temporary sensitivity occurs in 15–20% of patients post-treatment, manageable with desensitizing products.
- Complexity: Advanced cases require coordination with specialists like prosthodontists or endodontists.
Future Trends
Restorative dentistry is evolving:
- Digital Dentistry: CAD/CAM and 3D printing enable same-day restorations, reducing costs and wait times.
- Advanced Materials: Zirconia, lithium disilicate, and bioactive composites enhance durability and aesthetics.
- Regenerative Techniques: Stem cell therapies and bioactive scaffolds may promote natural tissue repair.
- Minimally Invasive Methods: Improved adhesives and techniques reduce tooth preparation.
Conclusion
Restorative dentistry rejuvenates smiles by repairing and replacing damaged or missing teeth, enhancing oral health, function, and aesthetics. From fillings to full mouth reconstructions, these treatments offer personalized, durable solutions. With proper care and innovations like digital dentistry and regenerative therapies, restorative dentistry ensures lasting results. Patients seeking to restore their smile should consult a certified dentist or visit American College of Prosthodontists for tailored treatment options.
